Select from the tabs below to see what services we offer
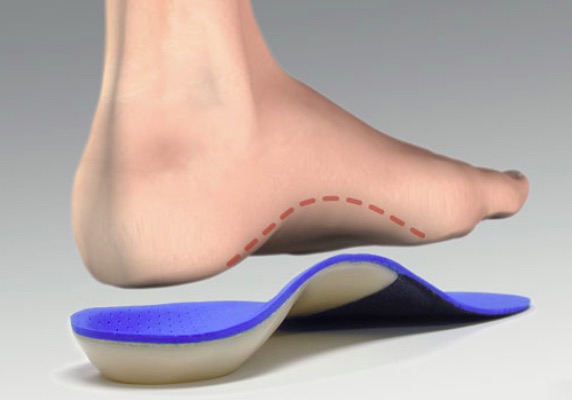
Foot Orthoses (FO’s)
Custom foot orthoses are medical devices prescribed by a foot and ankle specialist. These are different from basic shoe inserts and arch supports in that they have two functions. FO’s can be used to accommodate or offload a prominent area. This can be helpful for bursitis, calluses beneath bony prominences and ulcers. They can also help the foot function better in the case of hypermobility seen in tendonitis, fasciitis and other mechanically derived conditions. They can help support and align the foot and lower extremities as well for a more natural gait. It is important how the foot shape or mold is captured, whether it be via scan, foam box or making a plaster cast.
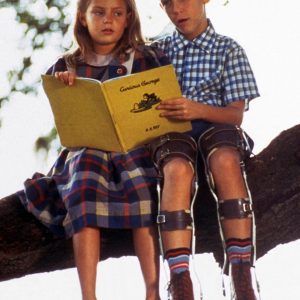
Orthotics can aslo help delay the need for surgery if it is not desired at a specific time or if a child must wait for growth plates to close and for his or her skeleton to be more physically mature. They can also help with pain following a surgery if an optimal result was not possible or achieved.
Orthopedic Shoe Modifications
Even after the ‘best fitting’ shoe is found, it still may not fit well enough for a successful orthotic treatment plan. The footwear may need further modifications that can be simple or complex.
Lift: Additional material is added either internally or externally to a shoe to add height to one side; this is usually applied when a structural leg length difference is determined.
Stretching: Stretching the upper of a tight-fitting shoe to offer more room can reduce painful pressure to a hammer toe or bunion; the use of a professional shoe stretcher, a wooden shoe stretcher, or a ball-and-ring stretcher can be helpful.
Resole: The original sole is removed and replaced to offer a level sole or different tread.
Buttress/ Flare: This is rubber material added to the outside of the shoe to bolster up the shoe support and offer a wider base of support.
Rocker sole: Your Orthotist can grind a smooth forward roll onto the shoe when your foot has limited or painful ROM at the forefoot
Shuffle plate/Toe slider: This is an addition of a smooth, low friction material to the bottom of the front of the shoe to reduce shoe gripping which can lead to falls. This is often used for stroke patients with foot drop.
Closure modification: This is a permanent external modification of the upper of the shoe to change its closure. Examples include the addition of hook-and-loop (Velcro) straps, buckles, or lacing changes such as lock lacing.
Excavations: This is a hole which is drilled out of the midsole of the shoe from the inside to create a well or hollow for a soft tissue lesion, bony prominence, or sensitive area.
Ankle Foot Orthoses (AFO’s)
An ankle-foot orthosis, or AFO, is a support intended to control the position and motion of the ankle, compensate for weakness, or correct deformities. AFOs can be used to support weak limbs, or to position a limb with contracted muscles into a more normal position. In addition, AFOs are used to control foot drop caused by a variety of neurologic and musculoskeletal disorders. Due to the common use for addressing foot drop, AFO has become synonymous with the term “foot-drop brace”.
The goal of AFO use is to stabilize the foot and ankle and provide toe clearance during the swing phase of gait. This helps decrease the risk of catching the toe and falling.
A typical AFO creates an L-shaped frame around the foot and ankle, extending from just below the knee to the tips of the toes. AFO’s are usually custom molded to an individual wearer or in some cases custom built around the wearer, and can be fabricated of a variety of materials, including heat-moldable plastics, metal, leather and carbon composite. AFOs are the most commonly used orthoses, making up about 26% of all orthoses provided in the Canada. Different AFO designs are intended to address specific purposes and can be separated into 3 main categories:
Carbon Composite/Flexible AFO’s
These orthoses are advanced AFO’s that use the principle of energy storage and return (ESR) to allow for a much more natural movement. More conventional AFO designs rely on completely blocking motion in certain directions to achieve their goal where flexible AFO’s rely on much lower forces of resistance to guide the ankle in the correct direction. This allows the user to make use of their full range of motion while getting the benefits of having their motion restricted in a dynamic fashion. These devices are more suited to patients who present with mild to moderate foot drop, those with variable requirements or those who require smaller corrective forces to help during gait.
Traditional Thermoplastic AFO
A thermoplastic AFOis a usually a custom fabricated, molded plastic device. It is designed to enclose the back of the calf and bottom of the foot, generally speaking and can be fabricated with or without ankle motion. They are typically used, fit into an existing shoe without modification to said shoe. A thermoplastic AFO is generally for patients that suffer from a neurological or orthopedic conditions. Some examples include: CVA (Stroke), MS (Multiple Sclerosis), CP (Cerebral Palsy), Traumatic Brain Injury, ALS (Amyotrophic Lateral Sclerosis). A Thermoplastic AFO is also an excellent choice if the patient requires extra ankle stabilization and protection against sprains in addition to the underlying issues. Patterns and colors are also readily available on thermoplastic AFO’s
Metal/Leather (Conventional) AFO
A conventional AFO is usually a double, upright, metal device, with a leather-covered band at the calf. The ankle joints may be adjustable to control ankle motion or assist with toe pickup. The joints attach to a metal stirrup that is fastened directly to the shoe, but may be attached to a removable plastic or metal footplate that slides into a shoe. A conventional AFO is often used where swelling of the leg and foot is present or there is a risk of sores on the foot. While still popular with some patients, this type of brace is becoming less popular as more modern and lighter designs become availlable.
Knee-Ankle-Foot Orthoses (KAFO’s)
A KAFO is a long-leg orthosis that spans the knee, the ankle, and the foot in an effort to stabilize the joints and assist the muscles of the leg. While there are several common indications for such an Orthosis, muscle weakness and paralysis of the leg are the ones most frequently identified. The most common causes of muscle weakness include, Poliomyelitis, Muscular Dystrophy, Multiple Sclerosis and Spinal Cord Injury,
Until recently, the best option for a patient with weakness of the muscles that control the knee was to wear a KAFO with a locked knee joint. This provided stability to the knee to prevent involuntary flexion, but caused other associated problems like muscle atrophy and increased energy expenditure in gait. Within the past few years, a newer design of knee joint has been developed that can automatically lock and unlock at the appropriate phases of the gait cycle to allow a more fluidic walking style. These knee joints can be used to create a KAFO that is appropriate for certain patients with knee weakness that fit the treatment criteria of the system.
Each KAFO is custom-made to the specific requirements of the individual. There are numerous design options available that make usage of the Orthosis both functional and comfortable. A detailed examination and assessment of the patient allows us to suggest the best available component combination.

-
KAFO’s come in many different shapes and sizes! Each brace is made to the exact specifications required by the user, and range from extremely solid, locked-knee to free motion and lightweight configurations. There are even some that utilize mechatronic/robotic knee and ankle joints to simulate actual human joint functions.
Conventional
Conventional KAFOs are custom made from a cast or tracing of the leg. These devices are made with metal and leather and attach directly to the shoe. Despite being a much older design and construction, they continue to be an option for patients who are accustomed to their fit and feel and can help some patients who have issues with the more intimate/enclosed fit of a more modern design.
Thermoplastic/Traditional KAFO’s
Thermoplastic/traditional KAFOs are custom made from a cast or tracing of the leg. They are custom made by first molding heated plastic (thermoplastics) to a modified replica of the leg. They have become popularized as a lighter and more cosmetically appealing design option, with a great many options for different levels of functionality and personalization. Although the majority are manufactured using Thermoplastics, they can also be manufactured using carbon fiber laminates.
Stance Control KAFO’s
Stance Control KAFOs are custom made from a cast or scan of the leg. These more advanced devices belong to a family of KAFOs that provide knee stability through “stance control”. The knee locks and unlocks to allow for a more efficient walking pattern, and in some cases, “smart orthoses” can provide variable resistance and/or functional assistance to movements as required in each individual case.
Spinal Orthoses
Spinal orthoses are used to treat patients with a variety of spinal disorders ranging from lumbar pain to complex spinal trauma and deformity. The primary goals of spinal orthoses are to aid a weakened muscle group, correct/support a deformed spine, and maintain the stability of a fractured spine. The orthoses can protect a body part from further injury or can correct the position of a body part and can be separated into:
Lumbo-sacral orthoses (LSO’s): Focus on immobilizing and supporting your lumbar spine.
Thoraco-lumbo-sacral orthoses (TLSO’s): Focus on immobilizing and supporting your thoracic and lumbar spine.
Cervico-thoraco-lumbo-sacral orthoses (CTLSO’s): Focus on immobilizing and supporting your cervical, thoracic and lumbar spine.
Cervico-thoracic orthoses (CTO’s): Focus on immobilizing and supporting your cervical and thoracic spine.
Cervical orthoses (CO’s): Focus on immobilizing and supporting your cervical spine.

-
Spinal orthoses come in many different shapes and sizes! There are many different configurations and designs that utilize different materials to give the required support and protection. Your doctor and orthotist will work together to work out which is the most appropriate based on your individual requirements.
LSO
LSO’s come in a variety shapes and sizes, from custom hard shell devices designed to deal with severe spinal trauma to elastic tensor belts designed to merely offer mild support , and everything in between. Many modern custom and semi-custom devices make use of pulley systems and multi-material design to achieve lightweight and flexible but solid support that is capable of handling anything but the most unstable fractures.
TLSO
TLSO’s also come in a variety of shapes and sizes, however they are typically custom fit to each individual regardless of support and vary greatly in shape, size and design based on their intended functions. Some common uses are to correct scoliosis, protect the spine post-surgery or to stabilize the spine immediately after a traumatic injury that does not require surgery. They can also be used to help with positioning a patient who has excessive weakness who would be unable to otherwise hold themselves upright.
CTLSO
CTLSO’s are only typically required in instances where stabilization of the whole spine is required, usually due to extreme trauma or multiple level surgery. These braces are almost always custom manufactured and require more rigid materials for manufacturing due to the strict immobilization which they are aiming to achieve.
CTO
CTO’s are used when only the upper 2 regions of the spine, the cervical and thoracic need to be immobilized and protected.
Upper-limb Orthoses
Upper-limb orthoses are designed to stabilize and immobilize the upper limb and prevent or correct joint contractures or formation of burn scar tissue. Orthoses will also promote healing, assist joint movement and reduce muscle spasticity when used appropriately.
They can be as small as a simple finger brace or extend all the way up to the shoulder depending on the needs of the patient, and can be manufactured using hard or soft materials depending on the desired characteristics and purpose of the brace. Some of the more common types of brace are listed below.
Wrist Hand Orthoses / Wrist Hand Finger Orthoses
WHO’s and WHFO’s are 2 of the most commonly seen upper limb orthoses.
WHO’s are often used to treat carpal tunnel syndrome or stabilize a fractured wrist and come in a multitude of different styles. They all share one thing however: they hold the wrist and hand in a fixed position or range of safe positions to prevent further problems developing or to correct an identified issue. However they do so, leaving the fingers free to use and as such are typically considered a more functional brace.
WHFO’s do all of the above, but include the fingers. These devices can either be static or dynamic. Static braces tend to treat high muscle tone or hold the wrist/hand/fingers in a safe position while at rest, whilst a dynamic brace would assist or augment the function of the joints allowing for greater overall function in a hand undergoing therapy or during rehabilitation.
Cranial Orthoses
Cranial orthoses are orthopedic helmets designed to achieve one of 2 goals: Protection or Correction. The two types of helmets are typically very different in their goals and applications and potential patients should be assessed by the orthotist prior to proceeding with treatment. Helmets can be a very effective treatment or safety tool and our experienced orthotists assess each patient on a case-by-case basis to ensure the correct course of action is being taken.
Helmets can be either prefabricated and then adjusted to fit, or custom made from a mold or scan taken using our on-site laser scanner. Below you can read a little about the different helmet types and when we use them.
Cranial Remolding Orthoses
Corrective helmets or Cranial Remolding Orthoses are designed to gradually change the shape of a child’s cranial bones by guiding bone growth in the appropriate regions. This is done to correct an abnormal shape as seen in Plagiocephaly or Brachycephaly. They DO NOT correct the cranial shape applying pressure to bend the bone into shape.
Each helmet is manufactured by taking a harmless laser scan of the infant’s head and then modifying the shape of the model to include space for the head to grow into over time. The helmet is worn for 23 hours per day and treatment is most effective when initiated at 5-6 months old, continuing until the cranial sutures have fused (around 1 year of age in most children). Cranial remolding helmets typically require close monitoring and regular adjustments as the child will be growing rapidly within the time-frame the helmet is being applied. Regular follow-up visits for adjustments and scans will ensure that the helmet is being effective without causing any discomfort.
Clinical Orthotic Consultants were the first in Ontario to adopt STARband as a treatment and have been successfully treating children with them for over 8 years now.
Protective Cranial Orthoses
Protective helmets or Protective Cranial Orthoses are designed to protect the head from impact trauma and can be either a hard or soft design.
Hard helmets are typically used in cases where someone has an unstable cranial fracture, has a section of bone removed from the skull or is at risk of severe penetrating impacts due to seizure or self harming behaviour. They provide a solid outer layer which prevents edge pressure from being focused at a single point on the skull and stops foreign objects from coming into contact with unstable or soft areas, while maintaining a soft inner padding to diffuse pressure from blunt trauma.
Soft helmets offer simple impact protection for blunt trauma from mild impacts and mild self-harming behaviour but does not protect against a more focused impact such as a table edge or doorframe.